Are You Prepared For The Pending Personalized Medicine Revolution?

By Rob Wright, Chief Editor, Life Science Leader
Follow Me On Twitter @RfwrightLSL

Arriving at 600 New Hampshire Avenue NW in Washington, D.C., I stride through the lobby of The Watergate toward the elevator. I am on my way to what promises to be a “lively” and “on-the-record” personalized medicine discussion hosted by the National Journal (a division of the Atlantic Media Company). Joining me this October evening are members of the medical community, media, a variety of healthcare experts, and three executives from the event’s underwriter, AstraZeneca.
Although my invitation provides a list of planned exploratory questions as well as a brief primer on personalized medicine, it is not until Dave Fredrickson, VP of specialty care for AstraZeneca, shares his opening remarks that I discern the desired outcome from the discussion. “Each of you represents different [personalized medicine] stakeholders,” he says. “We are keen on hearing your perspectives so we [AstraZeneca] know where to focus, so we are leaders in the field, not followers.”
The personalized medicine discussion is the third in a series of four involving topics on which AstraZeneca desires to have a leadership role. As the fourth has yet to take place, I am not at liberty to divulge the topic. However, the previous discussions focused on patient-centricity and value. And while there has been some media coverage, as well as blog postings on AstraZeneca’s Health Connections website of the previous discussions, these provided a somewhat surface-level understanding of the subjects. Given the enormous potential personalized medicine promises for patients, payers, providers, and pharma alike, there seems to be an opportunity to provide a much deeper understanding beyond the issues impeding progress. What follows are insights gained from diving deep into the world of personalized medicine — which will be nothing short of revolutionary.
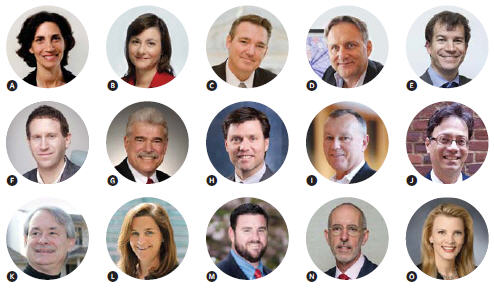
(A) Moderator Marilyn Werber Serafini Vice President, Policy, Alliance for Health Reform
(B) Julie Appleby Senior Reporter, Kaiser Health News
(C) Rich Buckley Vice President, North America Corporate Affairs, AstraZeneca, and President, AstraZeneca Healthcare Foundation
(D) Andrea Califano, Ph.D. Clyde and Helen Wu Professor of Chemical Systems Biology; Chair, Department of Systems Biology; Director, JP Sulzberger Columbia Genome Center; Associate Director, Herbert Irving Comprehensive Cancer Center, Columbia University
(E) Dave Fredrickson Vice President, Specialty Care, AstraZeneca
(F) Yuval Itan, Ph.D. Postdoctoral Associate, The Rockefeller University
(G) J. Leonard Lichtenfeld, M.D. Deputy Chief Medical Officer, American Cancer Society
(H) Daryl Pritchard, Ph.D. Vice President, Science Policy, Personalized Medicine Coalition
(I) William Mongan Vice President, Business Development, New Product Planning and Foundations Portfolio, AstraZeneca
(J) Aris Persidis, Ph.D. President and Co-Founder, Biovista
(K) James Salwitz, M.D. Clinical Professor, Robert Wood Johnson Medical School
(L) Wendy Selig President and Chief Executive Officer, Melanoma Research Alliance
(M) Paul Sheives, J.D. Director, Diagnostics and Personalized Medicine Policy, Biotechnology Industry Organization
(N) J. Russell Teagarden, DMH, RPh Senior Vice President, Medical and Scientific Affairs, National Organization for Rare Disorders
(O) Sheila Walcoff, J.D. Chief Executive Officer and Founder, Goldbug Strategies, LLC
IS PERSONALIZED MEDICINE PRECISION MEDICINE?
Prior to attending this discussion, attendees were provided the following definition for personalized medicine — “Getting the right targeted treatment to the right patient at the right time.” While somewhat accurate, according to dinner discussion attendee, Andrea Califano, Ph.D., professor of chemical systems biology at Columbia University, this definition, along with the term itself — personalized medicine — creates a common misunderstanding. “We talked to people on the street,” says Califano. “They tell you that personalized medicine is getting a drug that is ‘personalized’ to your particular type of disease.” Califano shares that Columbia has been doing a lot of “N-of-One” studies. “N of something means how many patients you need to have in a study for it to be statistically powerful,” he explains.
“We’re doing studies that consist of a single patient. Of course you have to do a lot of these [studies] in order to have statistical power, but each patient is treated individually.” At Columbia they are finding that personalized medicine doesn’t necessarily require personalized medicines. “We find that the drugs that would work in patients are very much the same across a large number of patients,” he says. “It's just that we don't know which patient should get which drug.” This is why Califano says you are seeing a shift away from the traditional research approach which views cancer tumors as padlocks, biomarkers as the keyholes, and the drugs which fit and open the lock as the cure. “We’ve come to realize that cancer is not a disease of the organ,” he shares. “It’s a disease induced by the genetic pathway.” As a result, researchers have been approaching cancer with a repertoire of drugs. “In very many cases, what we find is drugs that were never even thought to be used for cancer, let alone a particular type of cancer, are putting the patient-derived xenograft in regression, especially when used in combination with others,” Califano states. For example, thalidomide, originally developed and prescribed as a sedative (1957), is Celgene’s branded treatment (Thalomid) for multiple myeloma. Imatinib, first approved by the FDA in 2001 to treat patients with advanced Philadelphia chromosome positive chronic myeloid leukemia, today has 10 indications generating $4.6 billion+ in annual sales for Novartis under the brand names of Gleevec and Glivec.
These are just a few of the reasons why Columbia University is using the term “precision medicine” when referring to the concept of personalized medicine, and why the school has also created an interdisciplinary precision medicine task force. Consisting of nearly 40 faculty members located throughout the institution, the task force is taking a university- wide approach to precision medicine, rather than just a medical one owned by a single department. Daryl Pritchard, Ph.D., VP of science policy at the Personalized Medicine Coalition (PMC), feels that getting caught up in the semantic debate over which term is better (i.e., precision or personalized) will only further confuse patients. From the practicing clinician perspective of James C. Salwitz, M.D., clinical professor at Robert Wood Johnson Medical School, the belief is, “The bedside clinician doesn’t believe that personalized medicine is anything different than what they’ve been practicing for a long time. We need to start thinking of this at a much higher level, with the medical community having a holistic image of the patient, because what we are talking about is game changing.” Personally, I prefer the term personalized medicine. Here’s why.
WHO IS GOING TO PAY FOR OR REIMBURSE FOR PERSONALIZED MEDICINE?
One of the personalized medicine debates that elicited some strongly held opinions during the evening revolved around the question of who is going to pay for personalized medicine initiatives (e.g., genome sequencing, diagnostic testing) — with the patient being notably absent from the conversation regarding financial responsibility. J. Russell Teagarden, DMH, RPh, SVP medical and scientific affairs at the National Organization for Rare Disorders (NORD), commented, “They [patients] won’t pay for anything. They won’t pay for penicillin.” It is hard to argue with Teagarden, who spent 19 years developing policy coverage at Medco Health Solutions prior to joining NORD. He believes that patients have become so accustomed to having healthcare coverage that they don’t expect to ever have to pay much, if anything at all, and actually have to put forth effort into thinking that they may, should, or have to, on occasion, pay for healthcare. J. Leonard Lichtenfeld, M.D., the deputy chief medical officer for the American Cancer Society, referenced the experience of his spouse, a practicing OB/Gyn in Thomasville, GA, and her dealings with a Medicaid and uninsured patient population that is either unwilling or unable to pay for their healthcare.
JAMES SALWITZ, M.D.
Clinical Professor, Robert Wood Johnson Medical School
I find it unfortunate that we as a society have allowed the slow evolution of a healthcare insurance reimbursement system to devalue the products and services of payers, providers, and pharma alike to items of entitlement. Personalized medicine is what its name implies — personal — personal data and personal treatments. As such, there should be a reasonable portion of personal financial responsibility. While we can all probably point to some examples of individuals not wanting to pay for products or medical services, defining all patients in this way is a mindset in need of change — starting with all the stakeholders other than the patient.
There are numerous examples to dispute the notion of patients being unwilling to pay. For example, U.S. News & World Report notes the growing number of physicians moving away from accepting insurance to concierge care — cash-only and membership-based retainer models, even among primary care practices. During the discussion, Aris Persidis, Ph.D., president and co-founder of Biovista, a drug repositioning company, shared an example of patients being willing to pay. “There’s a company in Richmond, VA that is the eastern seaboard’s largest recipient of FedEx packages,” he states. “It’s called HDL – Health Diagnostic Laboratory.” According to Persidis, using technology to reduce the cost of the wet lab, combined with touting the ability to test for cardiovascular disease risk factors and some very simplistic correlations, HDL has grown into an enormous enterprise worth studying. While Lichtenfeld was quick to point out that HDL is under investigation for Medicare fraud, Persidis’ point wasn’t advocating the questionable behavior of HDL but the fact that many patients willingly paid for healthcare in the form of $120 diagnostic tests. Another example is the 23andMe direct-to-consumer personal genome test. While Paul Sheives, J.D., director of diagnostics and personalized medicine policy at BIO, stressed the limited viability of the do-it-yourself test, Wendy Selig, president and CEO of the Melanoma Research Alliance, questioned the ethics of such tests that give patients information about their susceptibility for getting a disease when a viable treatment does not presently exist. Nonetheless, Sheila Walcoff, J.D., CEO and Founder, Goldbug Strategies, a biomedical consulting firm, pointed out that over 700,000 people have already had their genome typed via the 23andMe retail DNA test. What makes this particularly interesting is when you consider 23andMe is just one company in a market expected to reach $19 billion globally by 2020. Despite 23andMe sales being slowed by FDA-imposed marketing restrictions, the impact of the product recognized by Time magazine as the best invention of 2008 in driving down diagnostic test prices is almost as glaring as the revelation that not only are people willing to pay outof- pocket for such tests but also share private medical information willingly and openly. Early in the personalized medicine discussion, Califano expressed one of his biggest concerns, saying, “We’ve actually been performing personalized medicine for maybe 100 years. Why is personalized medicine becoming such a hot topic at this point?” While Califano believes the cause to be the result of genome sequencing transforming scientific understanding of biology, Persidis, sees the consumer, not industry or the FDA, as being the driver that will tip personalized medicine from concept to reality. “I’m going to use the democratization of music as an example,” says Persidis. Though you may think this a silly comparison because healthcare is highly regulated, he reminded the group that music is regulated because it is considered intellectual property. “The consumer led the charge to change the rules,” he affirms. “What happened when music was democratized is that technology made it so darn easy and cheap, that the producers, along with everyone else, had to adapt.” Continuing he asks the group, “Can you imagine a world where it is so easy to have these [personalized medicine type] tests conducted, interpreted, and matched up with a person’s electronic medical record information, and then you extract the differential effect of drugs, possible benefits and risks, and a whole bunch of other things? This is possible today. If you stack all of the technologies we currently have together, you end up with a really cheap point-of-care solution that is good for the patient and the doctor.” If the cost can be brought down to a reasonable price point, patients most certainly will pay.
SHEILA WALCOFF, J.D.
Chief Executive Officer and Founder
Goldbug Strategies, LLC
CAN PERSONALIZED MEDICINE
BECOME A REALITY?
When the evening's moderator, Marilyn
Werber Serafini, VP of policy at the
Alliance for Health Reform, asked the
group what incentives and payments are
necessary to make personalized medicine
happen, James Salwitz, M.D., responded,
"As medicine is currently practiced, it can't
be done." There is a variety of reasons for
his well-placed skepticism. For the realization
of personalized medicine, a plethora
of interfaces needs to be developed
to facilitate the linking and sharing of all
your personal health data (e.g., electronic
medical health record, genome, medical
history, metabolome, microbiome, pharmacogenomics,
proteome, vitals), so it can
be properly analyzed. "If I were in the
drug development sector," Salwitz advises,
"I would invest in medical informatics."
Teagarden adds, "We don't have a uniform
payment system, but gazillions of different
payment systems, each having different
reasons for what they are willing to pay for
and why." The lack of uniformity across
insurances is one of the challenges he sees
to personalized medicine becoming a reality.
"Different payers from different segments
are willing to accept different levels
of evidence," he says. Sheila Walcoff sees
another obstacle, stating, "I think we're
at a crossroads for the two key pieces that
could prevent the promise of personalized
medicine — reimbursement and regulation."
Her concern is that if these two areas
aren't able to find an appropriate balance,
it will result in stagnation of innovation,
investment, and quality. Selig affirms,
"The incentives have to exist for people
to invest." Referring to the preclinical
space, she analogizes how the incentives are misaligned. "Industry is not investing
in preclinical because it's expensive and
hard to convince your shareholders it's
worth doing. Academia is doing it, but
under great duress due to funding constraints
and misaligned incentives which
emphasize publishing, not collaboration."
Yuval Itan, Ph.D., postdoctoral associate
at The Rockefeller University, agrees. "In
rare Mendelian [one gene] diseases, we are
becoming more efficient in actually identifying
the disease-causing gene," he states.
According to Itan, once they have proven
in the lab that a gene causes a disease,
and then they publish that finding, that's
where it typically ends. "For an academic
researcher there is usually no follow-up
as to the benefit of the discovery for the
patient," he laments.
All of these barriers considered, the personalized medicine revolution is coming, and probably sooner than you think. In an ironic stroke of luck, two days after attending the National Journal dinner discussion, I was invited to review The Personalized Medicine Revolution, a not-yet-released book by Pieter Cullis, Ph.D., professor of biochemistry and molecular biology at the University of British Columbia. He anticipates the impact of personalized medicine on you and how you live your life to be greater than any other technological advance you have ever experienced. While this may seem far-fetched, for those of us who experienced the world before the existence of the Internet, I am sure many of us would admit ever having envisioned how this once neat curiosity would absolutely change everything. But it took innovators and inventors to change the Internet from a cool interconnected computer tool used by researchers into something people could use as easily as any other home appliance. Cullis writes, "If you want to take advantage of the benefits of personalized medicine, you are going to have to start to assemble your digital self as best you can and use your doctor as a sounding board to help interpret what you find." This is the best businesspractice actionable information you have been waiting for. Because, though Persidis stated during the dinner that consumers will drive the personalized medicine revolution just as they did in music, it took the visionary leadership of Steve Jobs to bring all of the stakeholders together. If you want to be in the position of creating and shaping the iTunes of personalized medicine, you better figure out who are the leaders among key stakeholders and start bringing them together — now, before the likes of Google, Netflix, or some other revolutionary company does it for you. Rewards are not reaped by visionaries who lack the will to execute.
